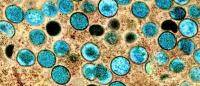
Your Questions About Monkeypox Answered
Monkeypox is not going to become the next COVID, but the outbreak has recently been declared a public health emergency in the United States and experts have expressed concern that the virus could become endemic.
The disease, which is caused by a virus, was first discovered in the 1950s in a colony of research monkeys in Europe (hence the name, monkeypox). The virus was eventually traced back to western and central Africa, where the first recorded human case was documented in 1970.
The virus occasionally infects people in Africa, particularly those who come in close contact with wildlife. This year, more than 1,700 cases have been detected in Africa, though more cases may have been unreported.
Though outbreaks outside of Africa have happened before—including in the United States—the current outbreak is the largest and most widespread. The official case count in the United States (as of Aug. 9) has risen to nearly 9,000, including more than 2,200 cases in the New York tri-state area, though these numbers are likely an undercount.
We spoke with Jason Zucker, MD, assistant professor of medicine in the Division of Infectious Diseases at Columbia University Vagelos College of Physicians and Surgeons, about monkeypox and what people in the United States need to know.
How worried should people be about monkeypox?
We are facing yet another significant public health challenge.
At the same time, monkeypox does not spread as easily as the coronavirus, which suggests it’s still possible to contain the outbreak.
How does monkeypox spread?
When you look at the epidemiological investigations that have been done—and monkeypox is not a novel virus, we have been following outbreaks for decades—the virus is spread primarily through direct skin-to-skin contact. It is possible for the virus to be transmitted in other ways, such as through contact with items like clothing and bed linens that were used by an individual with monkeypox virus or extremely close face-to-face contact with someone who has the disease, though this does not appear to be a significant driver of disease spread.
We’ll learn more with time, but the epidemiologic data we have on monkeypox does not support a link to airborne transmission as it did with the coronavirus, where we saw large increases in cases among health care workers and people who did not have close contact with each other. This means that an individual is unlikely to get monkeypox by being in the same room with someone who has the disease.
What signs and symptoms should people be aware of?
Monkeypox often starts with non-specific symptoms, things like fever, headaches, fatigue or feeling run down, and swollen lymph nodes in the groin. Within 5 days of these symptoms starting, patients develop a rash that can last for 2-3 weeks. The lesions can start on multiple parts of the body and progress through different stages until eventually scabbing over.
Monkeypox is a long disease. You can develop symptoms up to 3 weeks after being exposed. Patients are no longer infectious after their sores have scabbed over, those scabs have fallen off, and new skin has grown in its place. This process can take up to 4 weeks.
Though many of the pictures of monkeypox seen on the internet show the characteristic lesions, in this outbreak lesions have been presenting differently and often do not resemble those pictures.
This includes lesions primarily or only in the genital and perianal area and sometimes occurring without fever, headaches, or any of the other systemic symptoms. The lesions can easily be confused with herpes or syphilis lesions, which can also occur at the same time and can be extremely painful. This is a great reminder that you should go and see your doctor any time you have abnormal skin lesions.
Since thinking about monkeypox is relatively new for many U.S. providers, if you have lesions that are unusual to you, go see your doctor and ask them about monkeypox to help raise their suspicion. For clinicians, especially given the presentations during this current outbreak, it’s a great reminder about the importance of taking a good history, including a sexual history, and remembering to add monkeypox to your differential along with traditional sexually transmitted infections.
Who is at risk?
The vast majority of people who have been diagnosed to date with human monkeypox virus are self-identifying men who have sex with men. This is likely due to shared sexual networks. But just like other diseases, there's no reason it can't spread to other communities via sexual or other close contact.
We are just starting to see a small number of infections in women and children. It’s important to note that all of these patients had close contact with someone who tested positive for monkeypox. It’s believed the disease may be more severe in children under 8 and may lead to worse outcomes in pregnant women.
How can people avoid monkeypox?
It is important that we make sure that the communities currently at greatest risk are aware of this disease. The CDC has put out a document on social gathering, safer sex, and monkeypox, which has a lot of things that people can do to lower the chance of getting monkeypox. The most important step is to talk to your partners; find out about recent illnesses, ask about rashes, or sores, and check yourself and your partner out prior to sex. If you yourself have lesions, make sure they stay covered and see a clinician to figure out what's going on.
Testing is essential to protect individuals and their partners from monkeypox. I can’t emphasize enough that anyone who has symptoms or concerns should see a health care provider and get tested right away. Most urgent care facilities and many primary care physicians have the ability to test for monkeypox. It’s faster and more convenient to get tested there than going to the emergency room. Individuals in New York City who do not have a doctor and want to get tested or evaluated can call 311.
I encourage patients who are at high risk to check themselves regularly for lesions or early signs of infection. They should also have open conversations with their sexual partners and encourage them to check themselves as well. They should also avoid sexual contact while waiting for test results.
Can vaccination help?
We have been vaccinating people who may have been exposed to monkeypox, or who are close contacts of a person with monkeypox, with a vaccine approved for smallpox and monkeypox (the viruses are closely related). The sooner an exposed individual gets the vaccine the better but the goal is to give the vaccine within 4 days of exposure to prevent disease and between 4 and 14 days to reduce symptoms of the disease. If given more than 14 days after exposure, the vaccine can reduce symptoms though it may not be able to prevent the disease. This type of vaccination strategy has helped contain other outbreaks.
The vaccine takes 2 to 3 weeks to work, so just being vaccinated does not mean you don’t need to worry about monkeypox.
The vaccine—marketed as JYNNEOS in this country—is also available now to individuals at high risk of being exposed to monkeypox, even if they haven’t had a documented exposure to someone with monkeypox. This approach could help slow the spread of the disease in areas with large numbers of monkeypox cases. Side effects of this vaccine are minimal, including pain and swelling at the injection site. The other available vaccine, ACAM200, can cause fever, rash, and enlarged lymph nodes, and can’t be given to people with immune disorders, heart disease, and other disorders requiring treatment with steroids.
How is monkeypox treated and what’s the prognosis?
This outbreak is caused by the milder clade 3 strain, which has a much better overall prognosis than the clade 1 strain that originated in central Africa. Historically, the disease caused by the clade 3 strain has a 1% to 3% mortality rate; in the current outbreak, 10 deaths have been reported worldwide, including 5 in countries where monkeypox is not endemic.
The vast majority of our patients are receiving outpatient supportive care until their symptoms get better. However, we are seeing patients with extremely painful symptoms, including painful sores in the mouth and throat that make it difficult to swallow, genital lesions that can become infected, or extreme rectal pain, making it difficult to go to the bathroom. A small number of these patients have required hospitalization so they can get supportive care and manage their pain.
There are no medications developed specifically to treat monkeypox. However, there are novel antivirals for smallpox and other diseases that may be useful for people with monkeypox, and those might be options for some people.
One of these antivirals, tecovirimat (TPOXX) is now being used to treat patients with monkeypox. TPOXX is an oral medication that has been approved by the FDA for the treatment of smallpox and is currently available for free through the strategic national stockpile. The drug may be used to treat adults and children with monkeypox. Tecovirimat has fewer serious side effects than other antiviral medications used to treat smallpox. But because the drug hasn’t been studied in people with monkeypox, we can’t say how effective it may be in people with this disease. However, anecdotally, patients who are being treated with tecovirimat have reported a reduction in symptom severity. Recently, formal clinical trials evaluating the effectiveness of TPOXX in patients with monkeypox have been announced.
What role does stigma play in this outbreak?
One of the biggest surprises to me is just how much stigma and shame are associated with this diagnosis. In addition to stigma patients who are diagnosed with monkeypox must isolate at home for up to 4 weeks, so this disease is challenging not just from a medical, but also from a mental health standpoint. We need to offer patients mental health and other supportive resources after their diagnosis. Eliminating stigma is the only way to ensure that patients receive the care they need.
References
This article was originally published June 14 and was updated August 9.
