Study Shows Why Many Cancer Cells Need to Import Fat
Columbia and MIT researchers are revealing the surprising reasons why cancer cells are often forced to rely on fat imports, a finding that could lead to new ways to understand and slow down tumor growth.
The research, led by Dennis Vitkup, PhD, associate professor of systems biology at Columbia University Vagelos College of Physicians, and Matthew G. Vander Heiden, MD, PhD, director of the Koch Center at MIT, was published June 23 in Nature Metabolism.
Common nutrients we eat, like fat, and the oxygen we breathe, are likely to play an essential role in the growth of cancer cells.
Oxygen is most known for its role in making energy in the body; that is why when we exercise, we start breathing harder. Because many cancer cells live in oxygen-depleted environments, it is often assumed that their growth is limited by energy.
But oxygen also has a less celebrated role, and that is to provide oxidizing power for the chemical reactions driving synthesis of biomolecules necessary for building new cells. Many biosynthetic reactions require a co-factor called NAD+, and when oxygen is lacking, cells cannot regenerate growth-promoting NAD+. And their key synthetic reactions come to a halt.
The new study found, surprisingly, that hypoxic cancer cells usually have more energy than they need for growth. When the researchers provided cancer cells with extra nutrients for energy generation, the cells did not respond.
Instead, when researchers used various methods to unclog biosynthetic pathways inhibited by lack of oxygen, cancer cells robustly increased proliferation.
The researchers found that while various biosynthetic pathways are sensitive to oxygen availability, synthesis of fats was among the most affected. Fat molecules are used to create membranes of new cells, and fat synthesis is especially challenging for cancer cells that need to synthesize new membranes for their growth. Without access to oxygen, cells cannot adequately supply their fat synthesis pathways.
“What makes our result very counterintuitive,” Vitkup says, “is that fat synthesis is not considered to be a process requiring a lot of oxygen. But our experiments demonstrated that up to 30% of oxygen used by cancer cells is not for energy generation but for synthesizing fats.”
As a result of oxygen’s impact on biosynthesis, cancer cells growing in oxygen-limited environments are strongly dependent on the import of fats from the environment. This creates a crucial vulnerability for cancer cells, such that cutting their supply of imported fats may slow or stop cancer growth.
Vitkup’s team is now trying to identify the receptors that cancer cells use to import fats in different tumors and which receptors could be targeted by drugs. The study also suggests that changing the composition of fats in the diet may play a vital role in influencing cancer growth.
“We usually think of cancer as being driven primarily by genetic mutations, but for cancer cells living in challenging conditions, such as oxygen-starvation, their environment is equally important,” Vitkup says. “Mutations stimulating uptake of fats, for example, will only promote tumor growth if these fats are actually available in their environment.”
References
More information
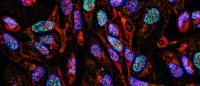
Photo of cancer cells growing in 2D by Nicola Ferrari / Getty Images.
The study, titled “Cancer cells depend on environmental lipids for proliferation when electron acceptors are limited,” was published in Nature Metabolism on June 23.
All authors: Zhaoqi Li (Massachusetts Institute of Technology), Brian W. Ji (Columbia and University of California, San Diego), Purushottam D. Dixit (Columbia and University of Florida), Konstantine Tchourine (Columbia), Evan C. Lien (MIT), Aaron M. Hosios (MIT), Keene L. Abbott (MIT), Justine C. Rutter (MIT), Anna M. Westermark (MIT), Elizabeth F. Gorodetsky (MIT), Lucas B. Sullivan (MIT), Matthew G. Vander Heiden (MIT), and Dennis Vitkup (Columbia).
The results published here are in part based upon data generated by the TCGA Research Network. This work was supported by the National Institutes of Health (grants R01CA201276, T32GM007367, U54CA209997, T32GM007287, T32GM007753, K99CA218679/R00CA218679, R35CA242379, and P30CA014051); the MD-PhD program at Columbia University; Damon Runyon Cancer Research Foundation; the Harvard/MIT MD-PhD Program; the MIT MSRP program; Lustgarten Foundation; SU2C; Ludwig Center at MIT; the MIT Center for Precision Cancer Medicine; Emerald Foundation; and Howard Hughes Medical Institute (International Student Fellowship and a Faculty Scholar award).
A.M.W. is a current employee of Revitope. M.G.V.H. is a consultant and scientific advisor for Agios Pharmaceuticals, iTeos Therapeutics, Droia Ventures, Faeth Therapeutics, Sage Therapeutics and Auron Therapeutics. All other authors declare no competing interests.