Some Brain Tumors May Respond to Immunotherapy, New Study Suggests
Immunotherapy has proved effective in treating a number of cancers, but brain tumors have remained stubbornly resistant. Now, a new study suggests that a slow-growing brain tumor arising in patients affected by neurofibromatosis type 1 (NF1) may be vulnerable to immunotherapy, which gives the immune system a boost in fighting cancer.
The findings, made by an international consortium led by researchers at Columbia University Vagelos College of Physicians and Surgeons, were published online today in Nature Medicine.
An estimated 100,000 individuals in the United States have NF1, a hereditary disease that can lead to the development of tumors throughout the nervous system, including a type of brain tumor called a glioma. Children usually have a slow-growing type of glioma, whereas adults often have a more aggressive type.
But whether slow-growing or not, gliomas are difficult to treat. Most are highly resistant to chemotherapy, and radiotherapy can aggravate, rather than relieve, symptoms, such as headaches and seizures. Since the tumors typically engulf delicate brain regions, surgery is rarely an option.
Immunotherapy has been successful for some patients with melanoma, lymphoma, and a few other types of cancer. But clinical trials have shown that, so far, it is ineffective for brain cancers in general.
Global Study Looked for Vulnerabilities in NF1 Brain Tumors
Surprisingly little was known about the molecular changes that occur in NF1 brain tumors, which has made it difficult to develop targeted therapies. In this study, researchers from 25 institutions around the world–led by Columbia’s Antonio Iavarone, MD, and Anna Lasorella, MD–performed an in-depth analysis of tumor samples from 56 patients to create the first comprehensive inventory of the genetic, epigenetic, and immune alterations in NF1 gliomas.
“This inventory will give us a much better idea of how to design individualized treatments,” Iavarone says, “but two findings from our study may have immediate clinical repercussions for NF1 patients.”
Many slow-growing NF1 gliomas appear susceptible to immunotherapy
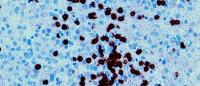
Immunotherapy is ineffective for most brain tumors because the tumors are infiltrated with large numbers of cells called macrophages that thwart the immune system’s attack.
The new study revealed that many slow-growing NF1 gliomas contain few macrophages and produce proteins, called neoantigens, that can trigger an immune system attack.
“We were surprised to find that approximately 50 percent of the slow-growing NF1 gliomas contained large numbers of T cells that have the ability to destroy cancer cells,” says Lasorella. These "high immune" tumors are good candidates for treatment with immunotherapy, which could unleash the T cells, and clinical trials are now being planned.
This study also discovered that a subgroup of brain tumors in patients without NF1 share the same molecular profile as the slow-growing NF1 gliomas. Future studies will have to establish whether these “NF1-glioma-like” brain tumors also exhibit the same immune features and are potentially vulnerable to immunotherapy.
Aggressive NF1 gliomas could be weakened with DNA-damaging drugs
Although aggressive NF1 tumors were packed with macrophages and are likely to resist immunotherapy, the researchers also found that many had a genetic defect that may leave them more sensitive to DNA-damaging therapies.
Cells in these aggressive tumors can reproduce, but the new cells contain many DNA errors. “If we treat the aggressive tumors with DNA-damaging agents, we might be able to introduce even more DNA errors that eventually prevent the cells from replicating and stall the growth of the tumor,” says Iavarone.
Radiotherapy and some current cancer drugs damage DNA, but drugs are also in development that may be more effective in cancer cells with this specific genetic defect.
References
Antonio Iavarone, MD, is professor of pathology & cell biology at Columbia University Vagelos College of Physicians and Surgeons, and a member of the Institute for Cancer Genetics at Columbia University Irving Medical Center.
Anna Lasorella, MD, is professor of pathology & cell biology and pediatrics at Columbia University Vagelos College of Physicians and Surgeons, and a member of the Institute for Cancer Genetics at Columbia University Irving Medical Center.
The full list of contributors is listed in the paper: “The molecular landscape of glioma in patients with neurofibromatosis.”
The study was supported by grants from the Children's Tumor FoundationSynodos Glioma Consortium (2015-04-007), the National Institutes of Health (R01CA101644, U54CA193313, R01CA131126, R01CA178546, R01CA179044, R01CA190891, and R01NS061776), and the Chemotherapy Foundation.
The authors declare no financial or other conflicts of interest.