Newly Found Genetic Variant Defends Against Alzheimer’s Disease
Discovery could launch new types of drugs to prevent, treat the disease
Columbia researchers have discovered a genetic variant that reduces the odds of developing Alzheimer’s disease by up to 70% and may be protecting thousands of people in the United States from the disease.
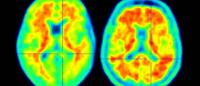
The discovery of the protective variant, which appears to allow toxic forms of amyloid out of the brain and through the blood-brain barrier, supports emerging evidence that the brain’s blood vessels play a large role in Alzheimer's disease and could herald a new direction in therapeutic development.
“Alzheimer’s disease may get started with amyloid deposits in the brain, but the disease manifestations are the result of changes that happen after the deposits appear,” says Caghan Kizil, PhD, a co-leader of the study that identified the variant and associate professor of neurological sciences (in neurology and in the Taub Institute) at Columbia University Vagelos College of Physicians and Surgeons.
“Our findings suggest that some of these changes occur in the brain’s vasculature and that we may be able to develop new types of therapies that mimic the gene’s protective effect to prevent or treat the disease.”
An attractive drug target?
The protective variant identified by the study occurs in a gene that makes fibronectin, a component of the blood-brain barrier, a lining surrounding the brain’s blood vessels that controls the movement of substances in and out of the brain.
Fibronectin is usually present in the blood-brain barrier in very minute amounts, but it is increased in large amounts in people with Alzheimer’s disease. The variant identified in the fibronectin gene seems to protect against Alzheimer’s disease by preventing the buildup of excess fibronectin at the blood-brain barrier.
"It’s a classic case of too much of a good thing,” Kizil says. “It made us think that excess fibronectin could be preventing the clearance of amyloid deposits from the brain.”
The researchers confirmed that hypothesis in a zebrafish model of Alzheimer’s disease and have additional studies in mice underway. They also found that reducing fibronectin in the animals increased amyloid clearance and improved other damage caused by Alzheimer’s disease.
“These results gave us the idea that a therapy targeting fibronectin and mimicking the protective variant could provide a strong defense against the disease in people,” says study co-leader Richard Mayeux, MD, chair of neurology and the Gertrude H. Sergievsky Professor of Neurology, Psychiatry, and Epidemiology.
The newest treatments for Alzheimer’s disease target the amyloid deposits directly and are very efficient at removing the deposits via the immune system. However, simply removing the deposits this way doesn’t improve symptoms or repair other damage.
“We may need to start clearing amyloid much earlier and we think that can be done through the bloodstream,” Mayeux adds. “That's why we are excited about the discovery of this variant in fibronectin, which may be a good target for drug development.”
Protective gene was found in people resilient to Alzheimer’s disease
The researchers discovered the protective variant in people who never developed symptoms but who had inherited the e4 form of the APOE gene, which significantly increases the risk of developing Alzheimer’s disease.
“These resilient people can tell us a lot about the disease and what genetic and non-genetic factors might provide protection,” says study co-leader Badri N. Vardarajan, PhD, assistant professor of neurological science (in neurology, the Gertrude H. Sergievsky Center, and the Taub Institute), who is an expert in using computational approaches to discover Alzheimer’s disease genes.
"We hypothesized that these resilient people may have genetic variants that protect them from APOEe4.”
To find protective mutations, the Columbia researchers sequenced the genomes of several hundred APOEe4 carriers over age 70 of various ethnic backgrounds, including those with and without Alzheimer's disease. Many participants were residents of Northern Manhattan who were enrolled in the Washington Heights/Inwood Columbia Aging Project, an ongoing study that has been conducted by Columbia University’s Department of Neurology for more than 30 years.
The study identified the fibronectin variant, and the Columbia team publicized their results in a preprint for other researchers to view. Based on the Columbia team’s observations, another group from Stanford and Washington universities replicated the study in an independent cohort of APOEe4 carriers, mostly of European origin.
“They found the same fibronectin variant, which confirmed our finding and gave us even more confidence in our result,” Vardarajan says.
The two groups combined the data on their 11,000 participants, which allowed them to calculate that the mutation reduces the odds of developing Alzheimer’s in APOE4 carriers by 71% and forestalls the disease by roughly four years in those who eventually develop the disease.
The researchers estimate that 1% to 3% of APOEe4 carriers in the United States—roughly 200,000 to 620,000 people—may also carry the protective fibronectin mutation.
Wide therapeutic potential
The fibronectin variant, though discovered in APOEe4 carriers, could protect against Alzheimer’s disease in people with other forms of APOE.
“There’s a significant difference in fibronectin levels in the blood-brain barrier between cognitively healthy individuals and those with Alzheimer's disease, independent of their APOEe4 status,” Kizil says.
“Anything that reduces excess fibronectin should provide some protection, and a drug that does this could be a significant step forward in the fight against this debilitating condition.”
References
More information
The study, “Rare genetic variation in Fibronectin 1 (FN1) protects against APOEε4 in Alzheimer’s disease,” was published online April 10 in the journal Acta Neuropathologica.
The research and researchers were supported by the Carol and Gene Ludwig Family Foundation, the Agouron Institute, the U.S. National Institutes of Health (grants R01AG067501, RF1AG066107, R01AG072474, R35GM148348, R01AG061796, U19AG074879, U01AG066752, U01AG046139, R01AG060747, P50AG047366, and R00AG075238), a Schaefer Research Scholars Award, Taub Institute Grant for Emerging Research (TIGER), the Thompson Family Foundation Program for Accelerated Medicine Exploration in Alzheimer’s Disease and Related Disorders of the Nervous System, and an Alzheimer’s Association Zenith Fellows Award.
Richard Mayeux, MD, is also director of the Gertrude H. Sergievsky Center and co-director of the Taub Institute for Research on Alzheimer's Disease and the Aging Brain at Columbia University Vagelos College of Physicians and Surgeons and neurologist-in-chief at NewYork-Presbyterian/Columbia University Irving Medical Center.
Other contributors and funding sources are listed in the paper.